Colorectal Quiz: July 17, 2023
Quiz for July 10th
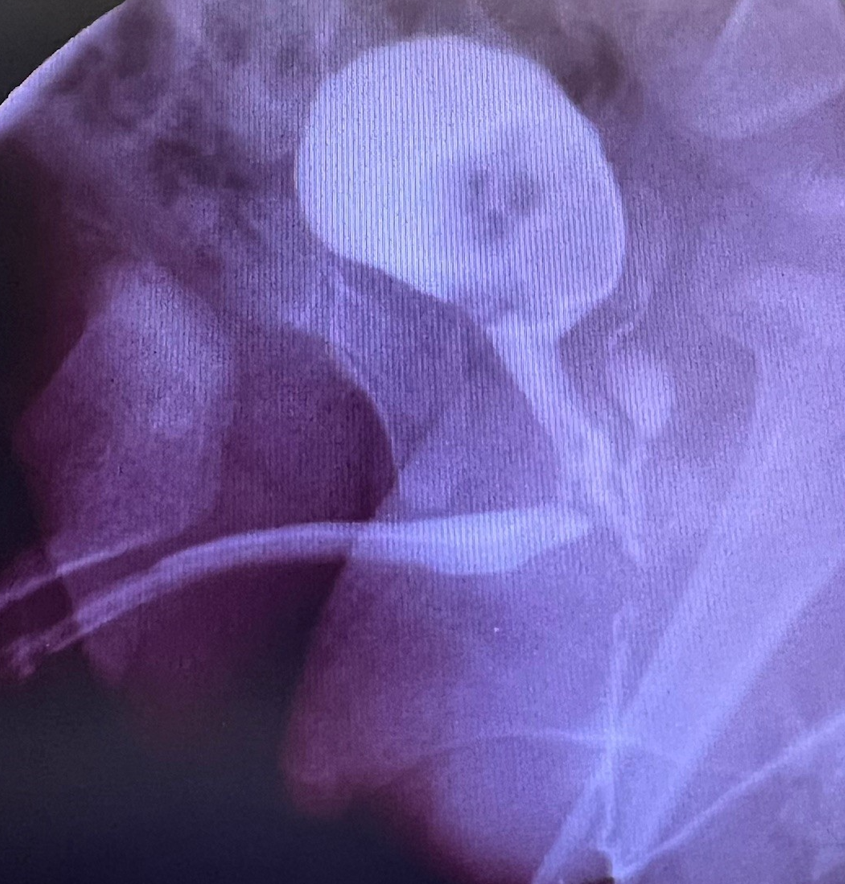
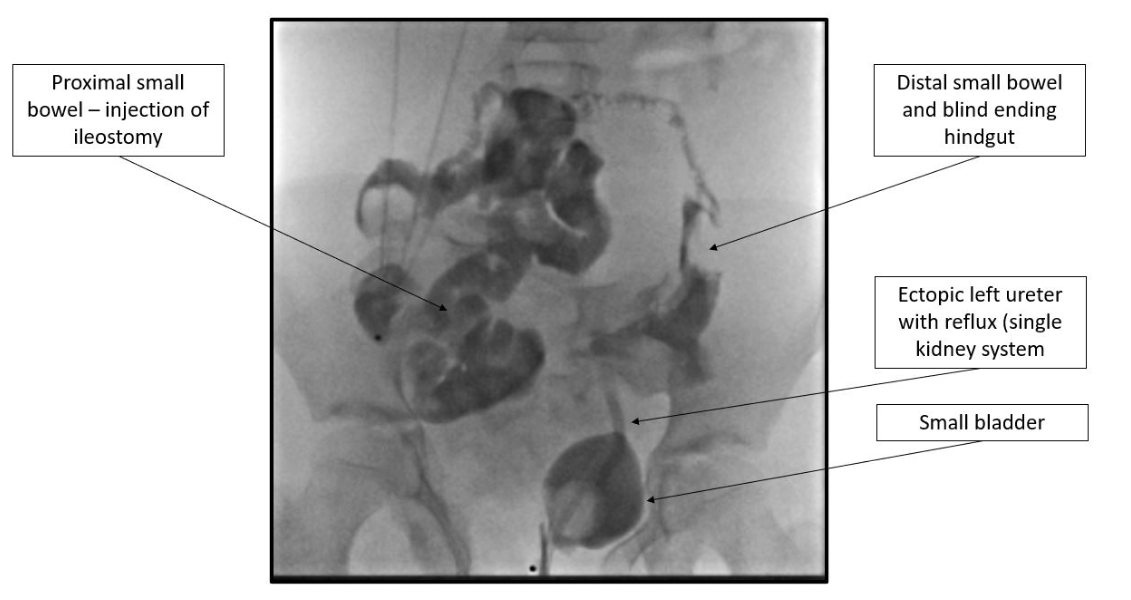
A 9-year-old born with covered cloacal exstrophy has been living her life with an ileostomy, which was done in the newborn period. She has been growing well. She leaks urine out the perineum at all times. The bladder neck is wide open on cystoscopy. The single perineal opening (the introitus) is good size and two cervices are visible. There is no anal opening, but she has good sphincteric contractions. A contrast study is shown below.
What would you offer this patient for a reconstruction?
Answer for July 10th
This patient is doing well with their ileostomy and appears to have distal ileum plus a large segment of hindgut, never used and not connected to the bladder. The bladder is quite small. I would recommend a bladder neck closure with bladder augment and Mitrofanoff, and for the colon to pull-through the segment of colon and make a Malone or a neoMalone.
Quiz for July 17:
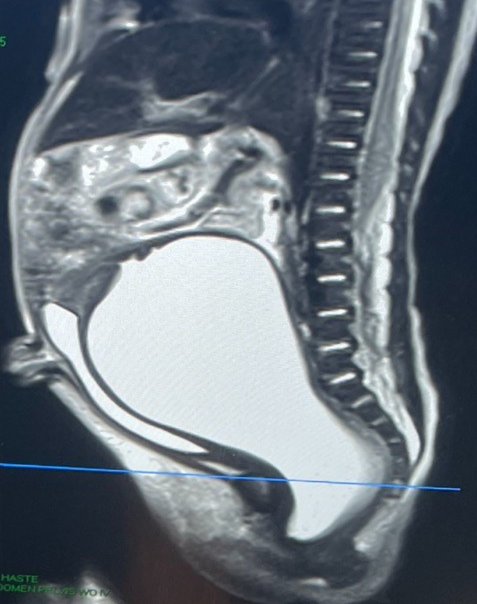
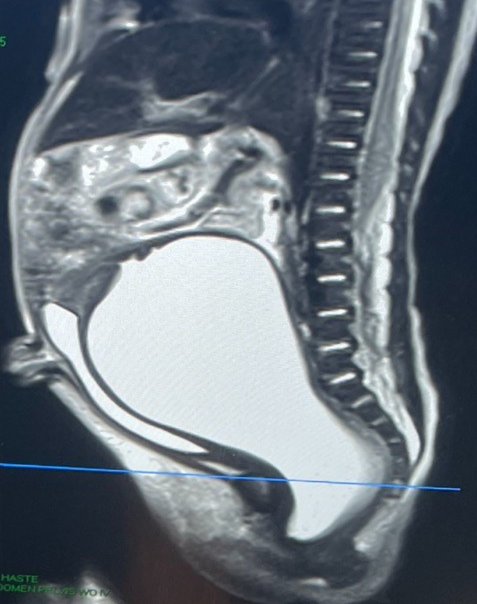
Here is the distal colostogram from an ARM patient who underwent a newborn colostomy.
What is the malformation and what would be your approach?

How would you handle this case?