CONDITIONS
ANORECTAL MALFORMATIONS
(ARM)
-
OVERVIEW
An anorectal malformation or ARM is a birth defect.
- It occurs early in pregnancy and affects the development of the rectum and anus.
- With this defect, the baby’s anal opening (where stool exits) and the rectum (the last part of the large intestine) do not develop properly.
- The defect prevents a child from having normal bowel movements.
- Anorectal malformations range in complexity and may occur at the same time as other abnormalities.
-
EVALUATION & TREATMENT
After birth, babies are examined to ensure the newborn’s anus is open and in the correct position. If the anal opening is absent or in the wrong spot, the doctor will look for stool coming out of the urethra, vagina, vestibule (area between the labia behind the vaginal opening), or skin near the expected anal position (usually in front of the typical location) within the first 48 hours after birth. If stool passes from an abnormal location or no anus is identified, the doctor will do a number of tests to understand the anorectal abnormality better. Sometimes an x-ray done in the newborn period shows the rectum is close to the skin surface and can be reconstructed. When the rectum is higher, a diverting colostomy is needed so that stool can pass through an opening in the abdomen, and the child can be fed. This surgery usually happens in the first day or two after birth. A colostomy connects the end of the colon to the skin of the abdominal wall to allow stool to pass into a pouch outside the body. A mucous fistula is created during the same operation. A mucous fistula attaches a disconnected part of the intestine to a surgically created small opening on the belly's skin (stoma). This connection helps people with certain bowel diseases pass mucous (intestinal secretions) out of the stoma instead of the anus. The child will go home to recover from this operation.
After the creation of a colostomy, a special x-ray is often done. It is called a distal colostogram. It creates a detailed image of your child’s organs. The image helps the surgeon identify the type of ARM. Once the ARM is identified, surgical planning to correct the problem will begin. Depending on the child’s anatomy, there are a few general courses for surgery. Reconstruction may be delayed until 1-3 months of age or when other associated medical conditions have been treated. Throughout the process, the surgical teams will coordinate the child’s care. Parents will receive education on how to help their child recover.
The following are some ARM types and surgical approaches that might be taken:
Incorrect location of the anal opening in the skin on the bottom with draining stool:
- In this case, a single operation can be performed to create an anal opening in the correct position. This procedure often occurs within a few days to a few months after birth.
Rectum does not reach the skin but is found low, near the anal sphincter:
- A single operation can be performed to create an anal opening in the correct position. This procedure often occurs within a few days of birth.
- Alternatively, this may also be treated initially with a colostomy to allow stool to pass. The corrective surgery would then be delayed for several months.
Rectum does not reach the skin and is not present near the anal sphincter:
This is a more complex malformation. The complete surgical repair will be done in different stages. Typically, the baby is allowed to grow in order to make the surgery easier and safer.
- After the distal colostogram is performed and the surgeon knows the rectal anatomy, a second operation will detach the rectal connection (fistula) from the genitourinary tract and will create an anal opening in the correct location. The colostomy will be left intact at this operation and not closed. This will allow the new anal opening to heal adequately. The child will go home to recover from this operation.
- The third operation will close the colostomy. This will occur a few months after the new anus is well healed.
Associated Anomalies
Children may also need surgery for associated anomalies or malformations during this time. The timing of the repair of both the anorectal malformation and other associated anomalies will depend upon the individual child’s situation.
Newborns with an ARM are also screened for other related health problems, called “associated anomalies,” which may involve the heart, reproductive system, and spinal cord. These studies may include the following:
- Abdominal and kidney ultrasounds to examine the urinary tract closely. Doctors look for blockages or abnormal fluid collections. Sometimes an additional test, a voiding cystourethrogram (VCUG), will be performed to examine the urinary tract further. In girls, an ultrasound will also be done to evaluate the vagina and uterus.
- Spinal ultrasound is used to look for a tethered spinal cord. An untreated tethered cord can lead to neurologic problems, such as bowel or bladder problems and leg weakness, as the child grows.
- If the spinal ultrasound shows any problems, an MRI of the spine will be performed when a child is 3-6 months old. The spine MRI will help explain the baby’s anatomy.
- An echocardiogram may be used to look for any heart defects.
- An x-ray of the sacrum shows how well-developed this bone is, which can be correlated with how well the pelvis has formed (including the muscles and nerves needed for continence). A sacral ratio can be calculated which helps with this assessment.
-
CONDITIONS ASSOCIATED WITH ARM
Some babies with birth defects in their anal opening (or ARM) have other health problems. VACTERL is an acronym that describes the problems that are sometimes found together.
VACTERL problems include:
V: Vertebral (including bony spine and/or the spinal cord)
Vertebral problems can include bony abnormalities seen on x-ray that may not cause long term problems or may result in scoliosis if missing vertebrae (bones) or parts of vertebrae occur. Sometimes, the sacrum does not form correctly which can cause the nerves that control urinary and bowel function to also form incorrectly. The spinal cord can also be affected by these abnormalities or may become attached to the base of the spine. These abnormalities need to be evaluated by a neurosurgeon. Surgery may or may not be required.
A: Anus (anorectal malformation)
Anorectal malformations see the discussion in the Evaluation & Treatment section.
C: Cardiac (heart)
Congenital heart defects are a common major birth defect associated with anorectal malformations. A cardiologist will evaluate the type and severity of a cardiac defect.
T/E: trachea (windpipe)/esophagus (swallowing tube)
Esophageal atresia is when the esophagus, or feeding tube, grows in separate pieces and does not connect to the stomach. Without a working esophagus, it's impossible to receive enough nutrition by mouth. A Tracheoesophageal fistula (TEF) is when there is an abnormal connection between the esophagus and the trachea, or windpipe. As a result, swallowed liquids or food can be inhaled into the lungs. To rule out these defects, a doctor inserts a thin tube fitted with a small light and camera into a child’s airway. This allows them to study the esophagus and the trachea.
R: Renal (including kidney, bladder, and reproductive organs)
Urinary tract abnormalities are noted in approximately half of children born with anorectal malformations. At birth the external genital and urinary organs will be examined to look for problems. If external abnormalities are found, an ultrasound is performed to assess for potential internal problems. These can include malformed or missing kidneys, abnormal fluid collections, or signs of poor kidney drainage. If abnormalities of the urinary system are noted at birth, often a special X-Ray called a voiding cystourethrogram (VCUG) will be performed. Close follow-up, often with repeated ultrasounds, is needed as the child grows. See the Internal Female Structural Anomalies section below.
L: Limbs (including arms and/or legs)
Limb abnormalities can include absent or displaced thumbs, extra digits (polydactyly), a fusion of digits (syndactyly), and forearm defects.
Internal Female Structural Anomalies
The internal female reproductive structures (fallopian tubes, uterus, cervix, and upper vagina) develop at the same time and place as the gastrointestinal tract and kidneys. So, girls with anorectal malformations have an increased chance of having a difference in these internal reproductive structures. There are many types of differences in development as seen HERE. Of note, the ovaries develop from a separate process, so they function as expected- producing hormones for puberty and ongoing periods as well as eggs for fertility. As your child grows, the gynecology team will gather information through exams (while awake and sedated) and imaging (like ultrasounds and sometimes MRIs) to help determine your child’s reproductive structures. Sometimes, gynecologic procedures or surgeries are offered or recommended, but this is not always needed and can sometimes be delayed until the patient is ready to make that decision. By the time your adolescent is ready to transition to adult health care providers, the gynecology team will ensure that the patient and their caregivers fully understand their anatomy and how it functions.
-
OUTCOMES
The long-term outcome of caring for an ARM patient includes successful management of constipation and the ability to achieve bowel control/continence.
Complications of surgery for ARM can include:
• Narrowing of the anoplasty (stricture)
• Prolapse (protrusion of the inner wall of the rectum) of the anoplasty
• Mislocation of the anoplasty (anus is placed outside the sphincter muscles)
• Separation of the incision or dehiscence
• Infection
-
AREA OF STUDY
The PCPLC registry collects data for patients with anorectal malformations and other conditions enrolled at member institutions.
Collecting data from multiple hospitals helps improve the care provided to patients. The data is studied to identify the best practices for caring for patients with ARM.
The data includes information such as testing, associated anomalies, details of surgical repair, hospitalizations, complications, and long-term bowel and bladder function.
Initial ARM studies using the PCPLC registry data have looked at prenatal factors in patients with ARM and strategies to help ARM patients achieve bowel control. PCPLC studies on ARM can be found on our Research & News webpage.
What is an Anorectal Malformation?
Slide title
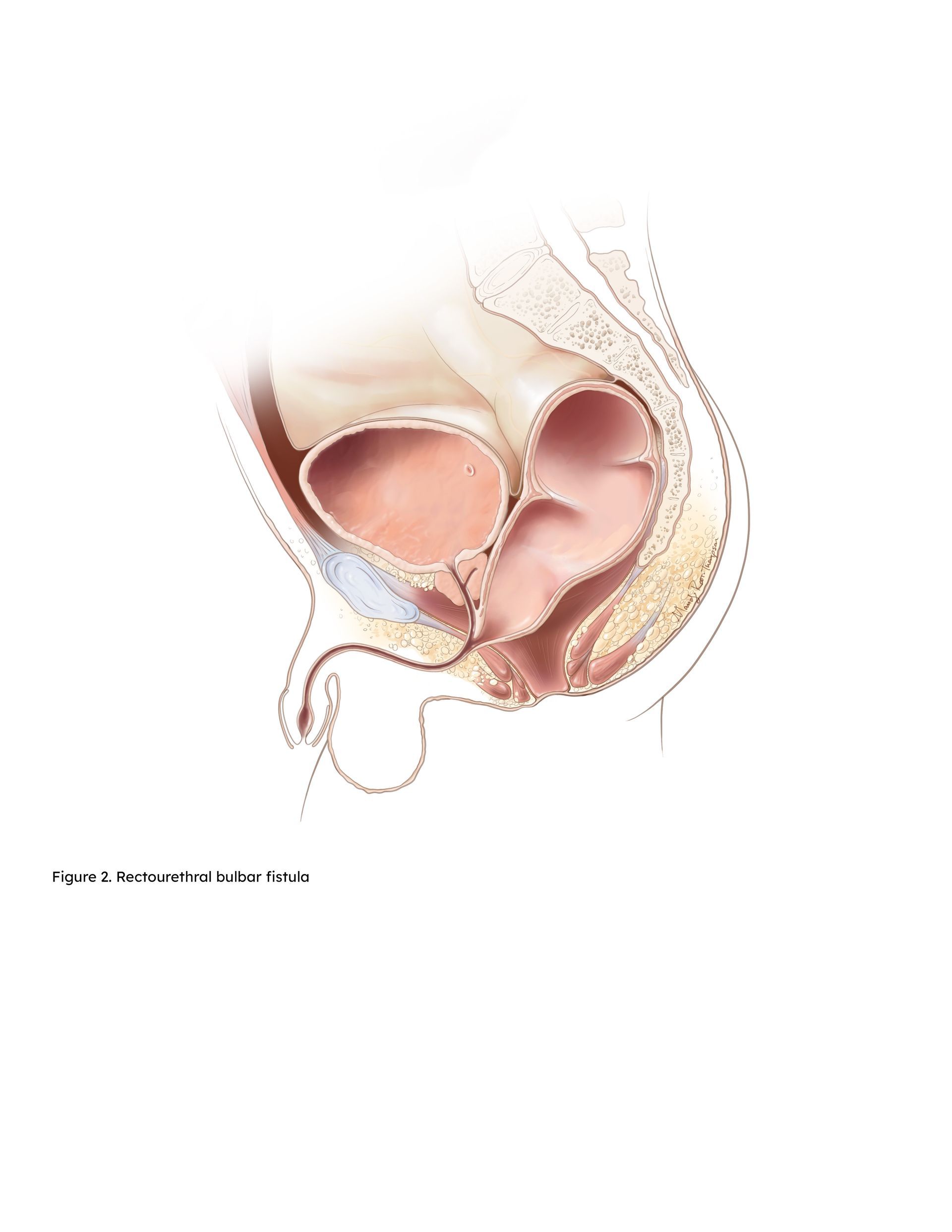
Rectourethral bulbar fistula
Button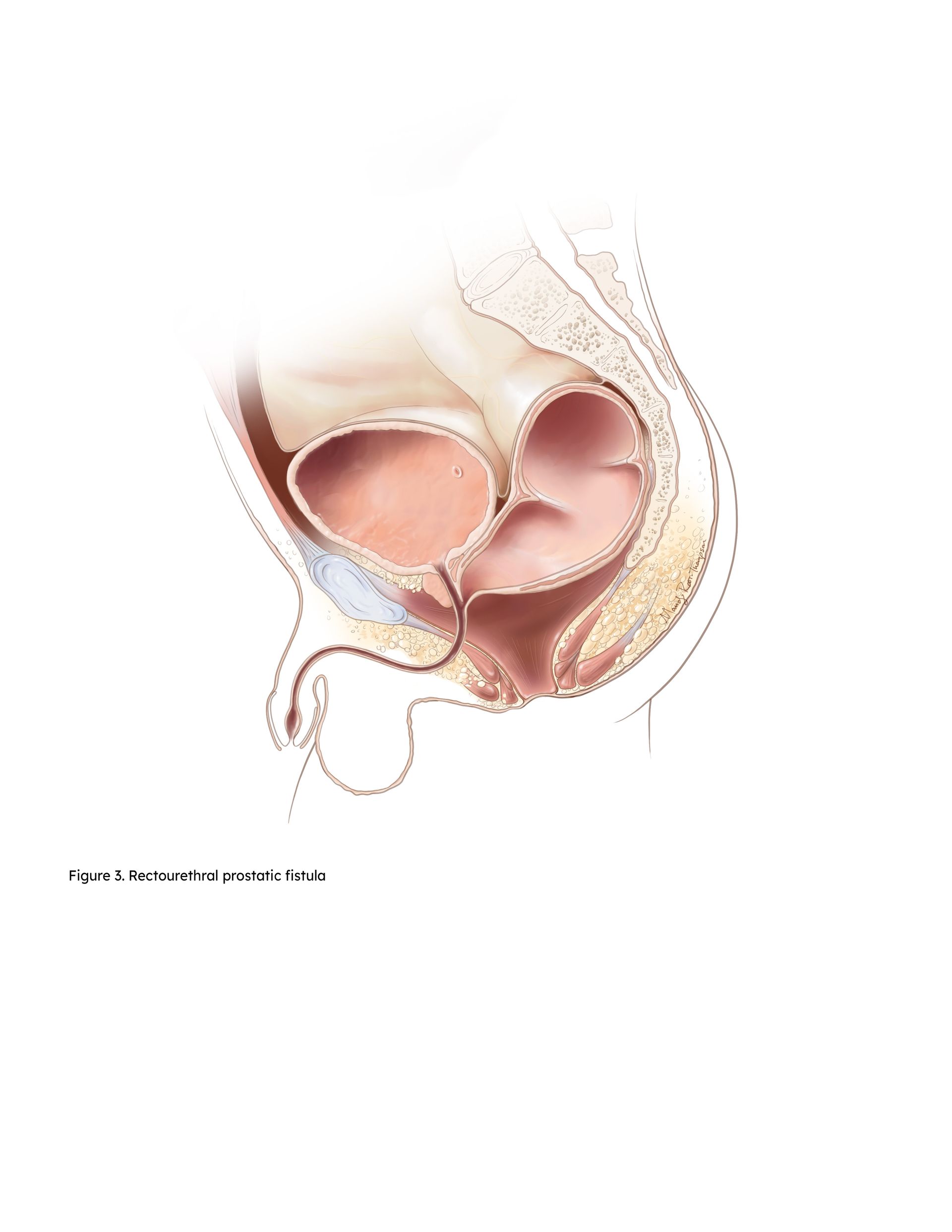
Slide title
Rectourethral prostatic fistula
Button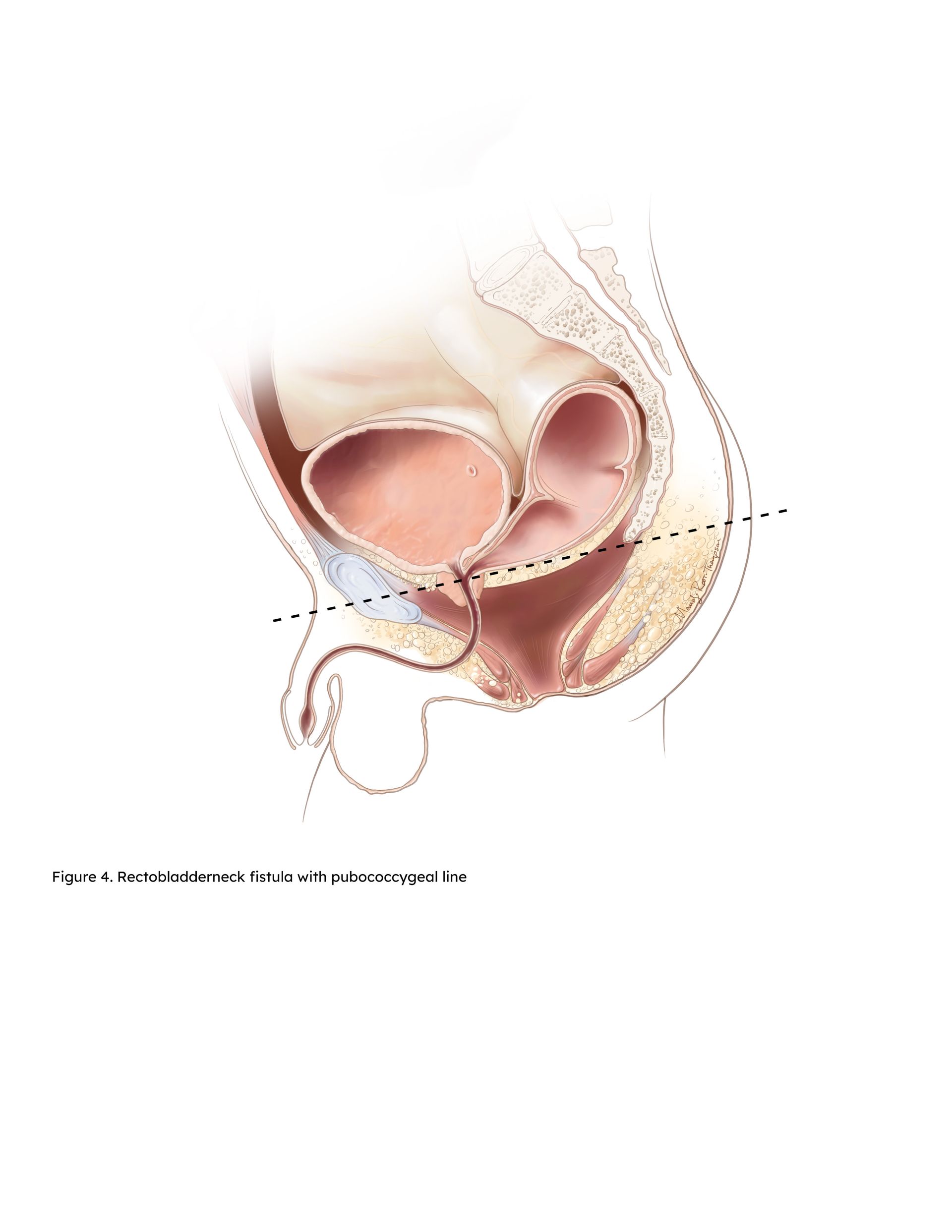
Slide title
Rectobladderneck fistula
Button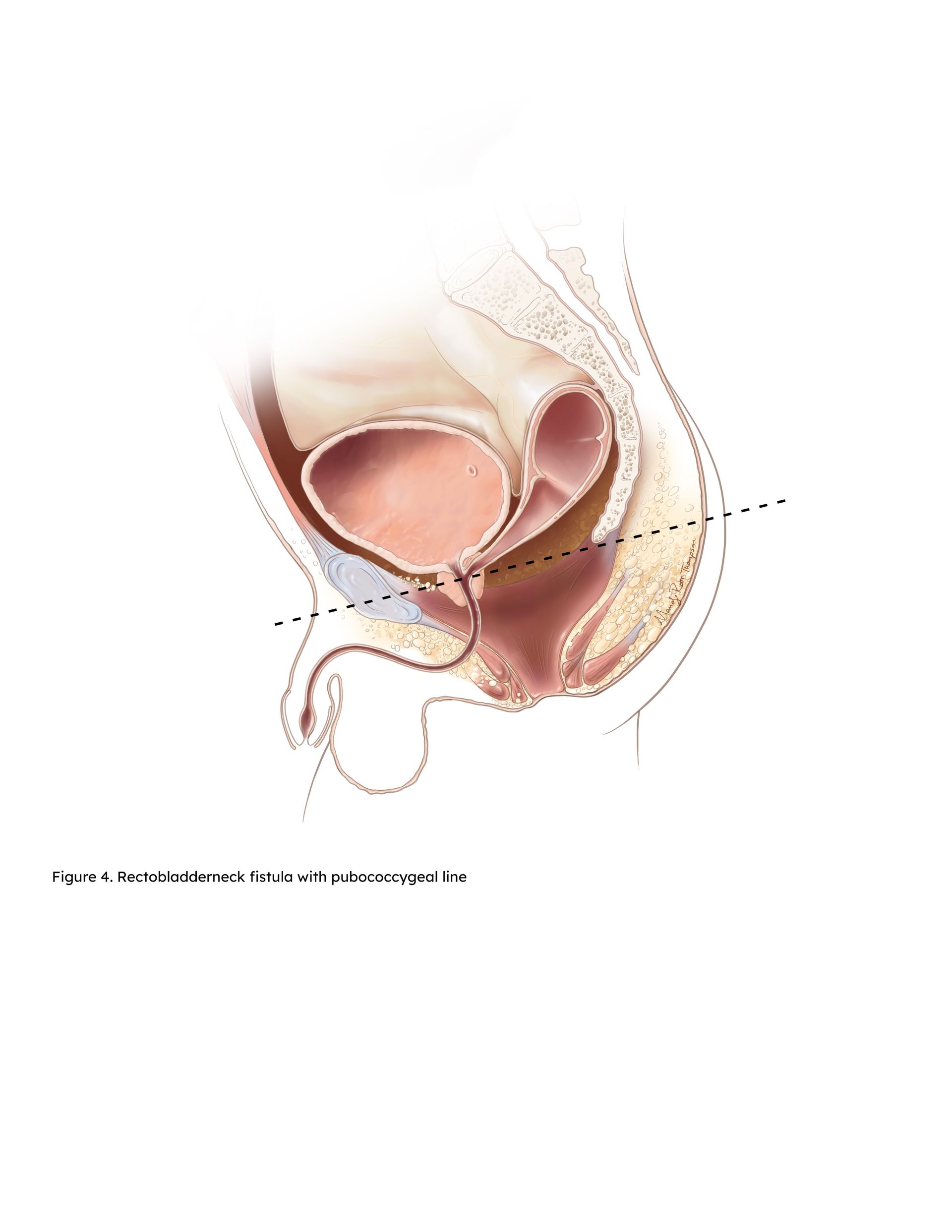
Slide title
Rectobladderneck fistula
Button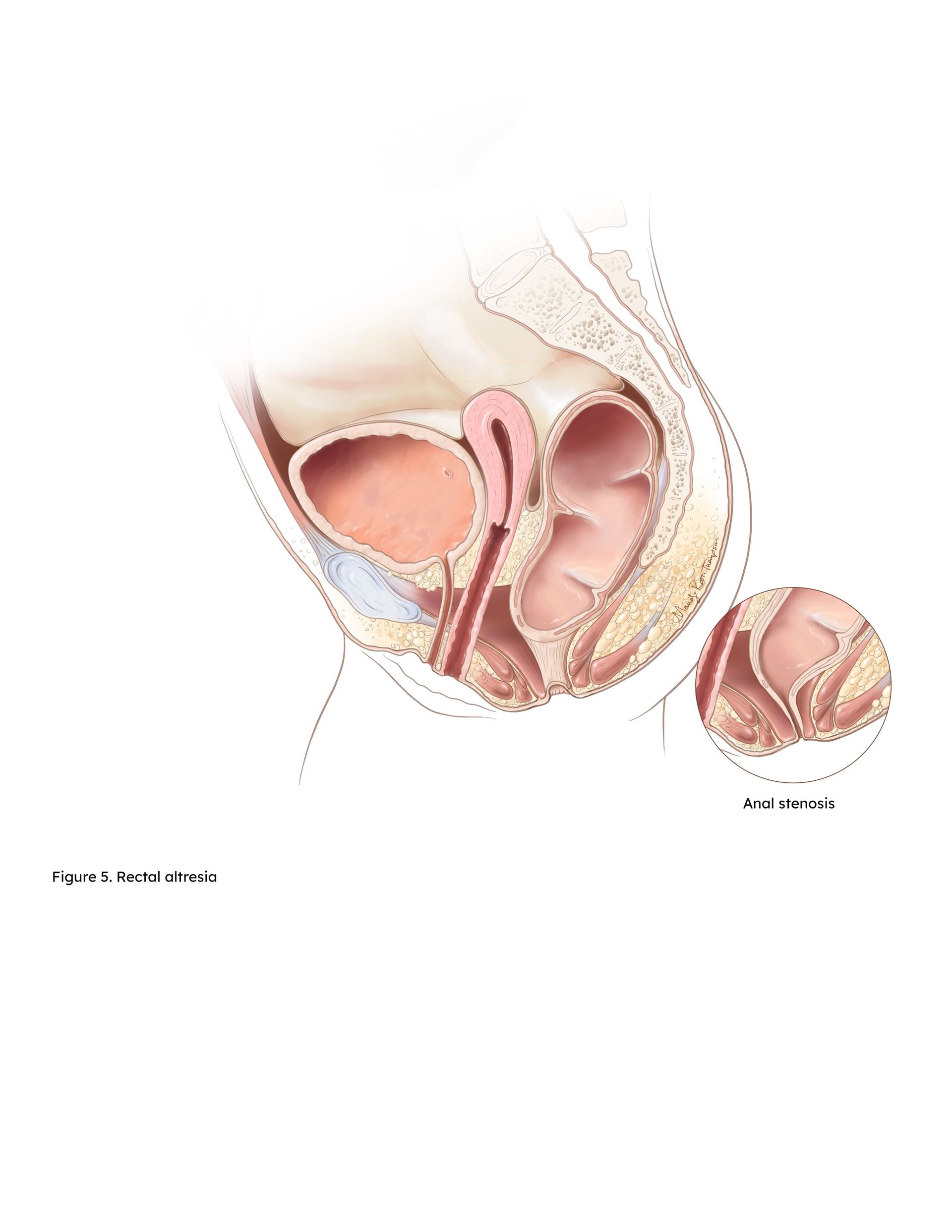
Slide title
Rectal Altresia-Stenosis
Button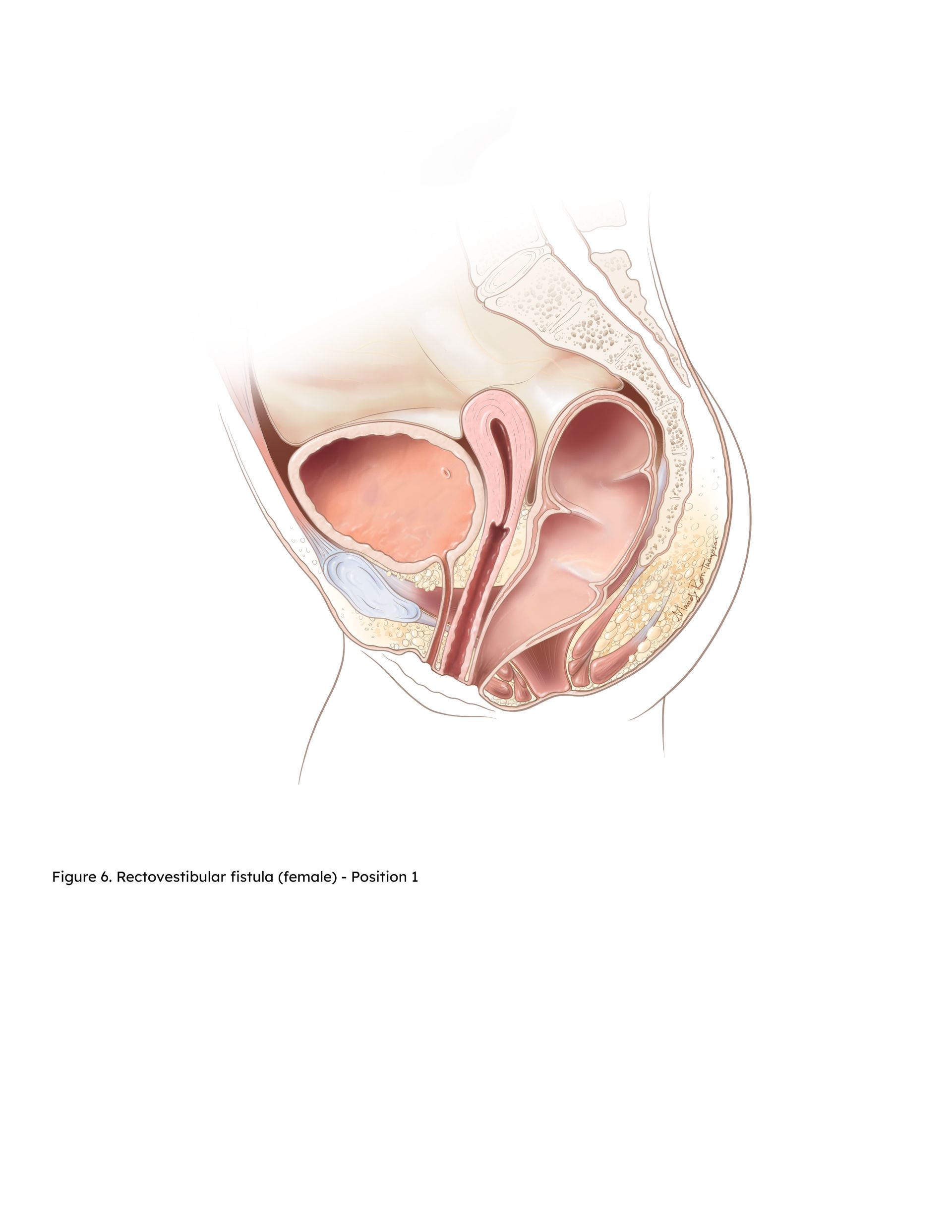
Slide title
Rectoperineal fistula - Position 1
Button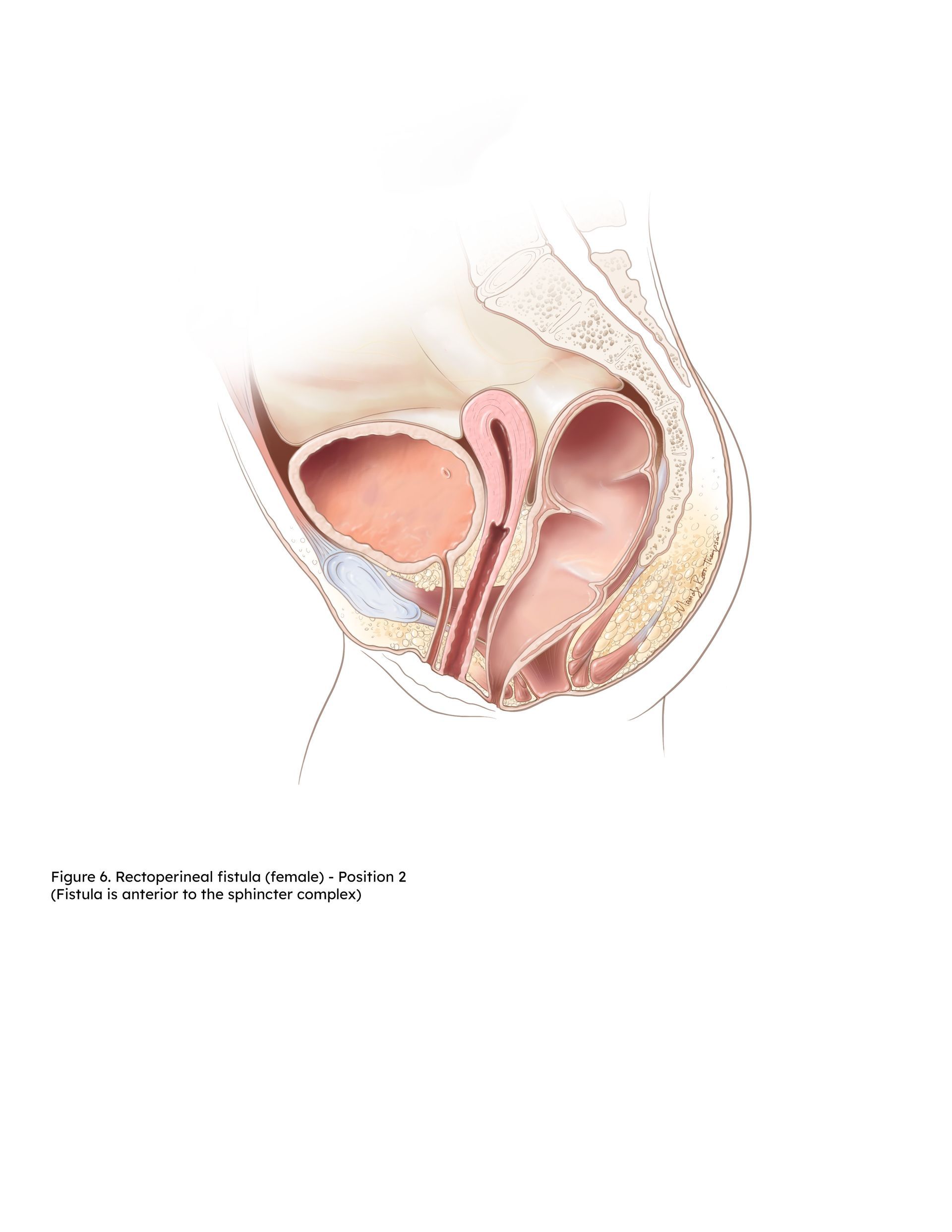
Slide title
Rectoperineal fistula - Position 2
Button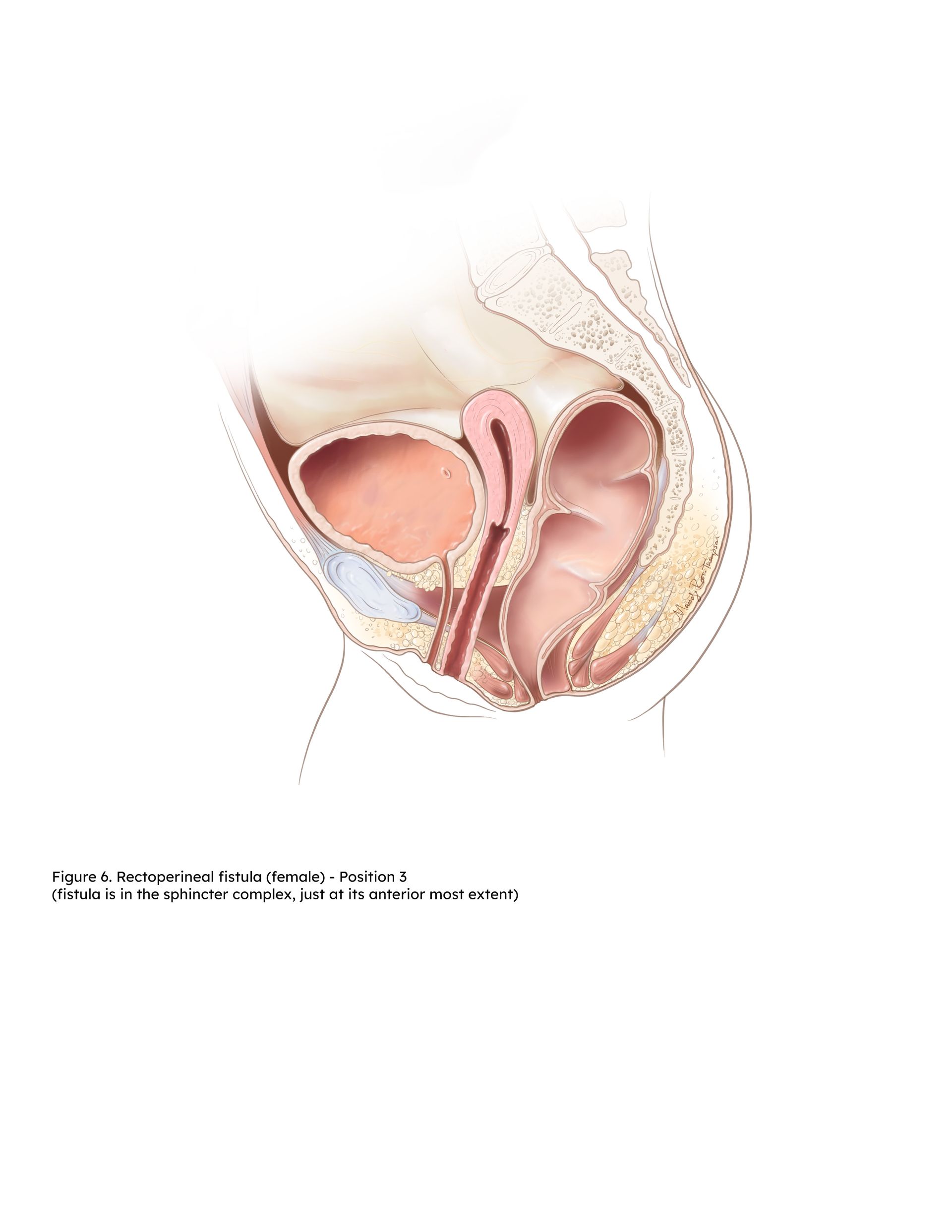
Slide title
Rectoperineal fistula - Position 3
Button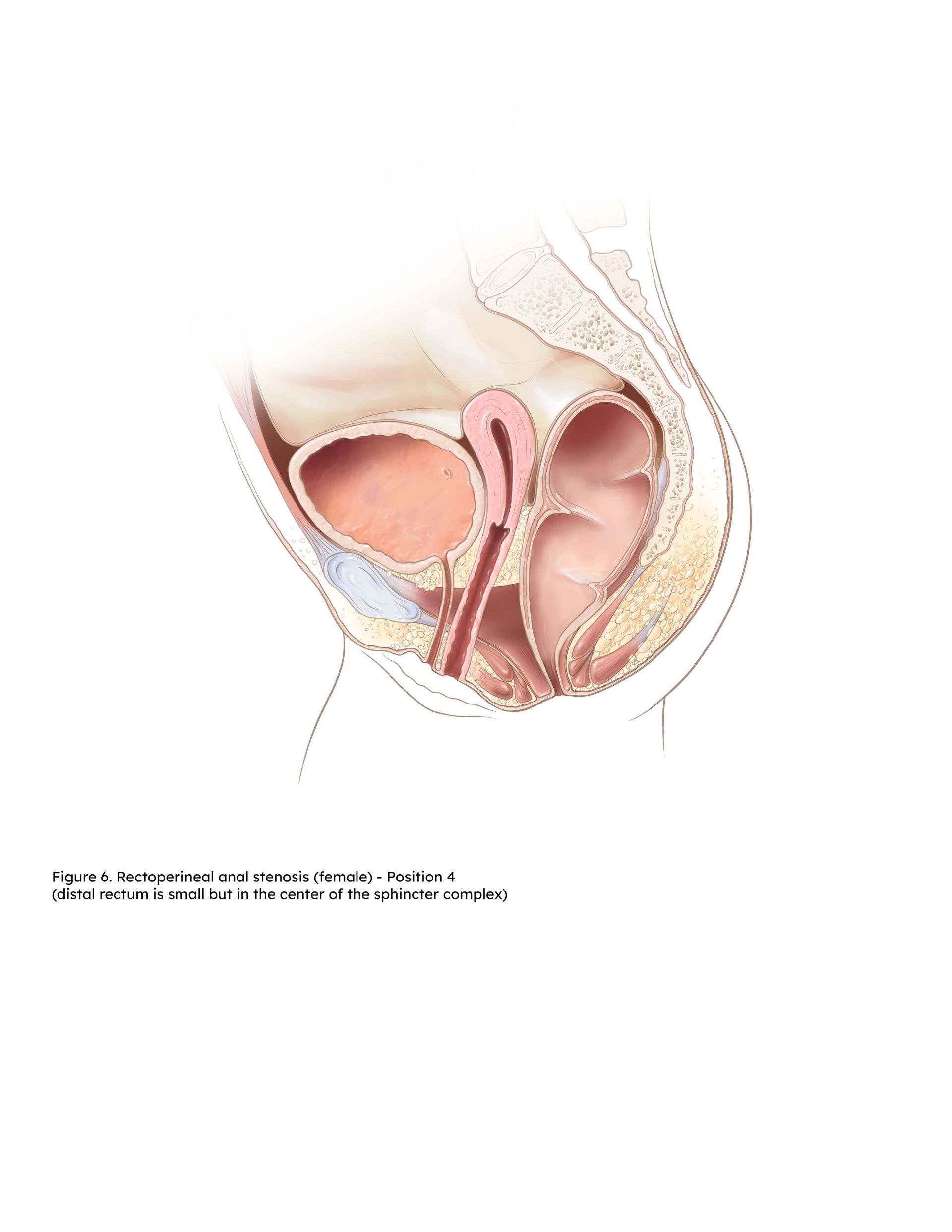
Slide title
Rectoperineal fistula - Position 4
Button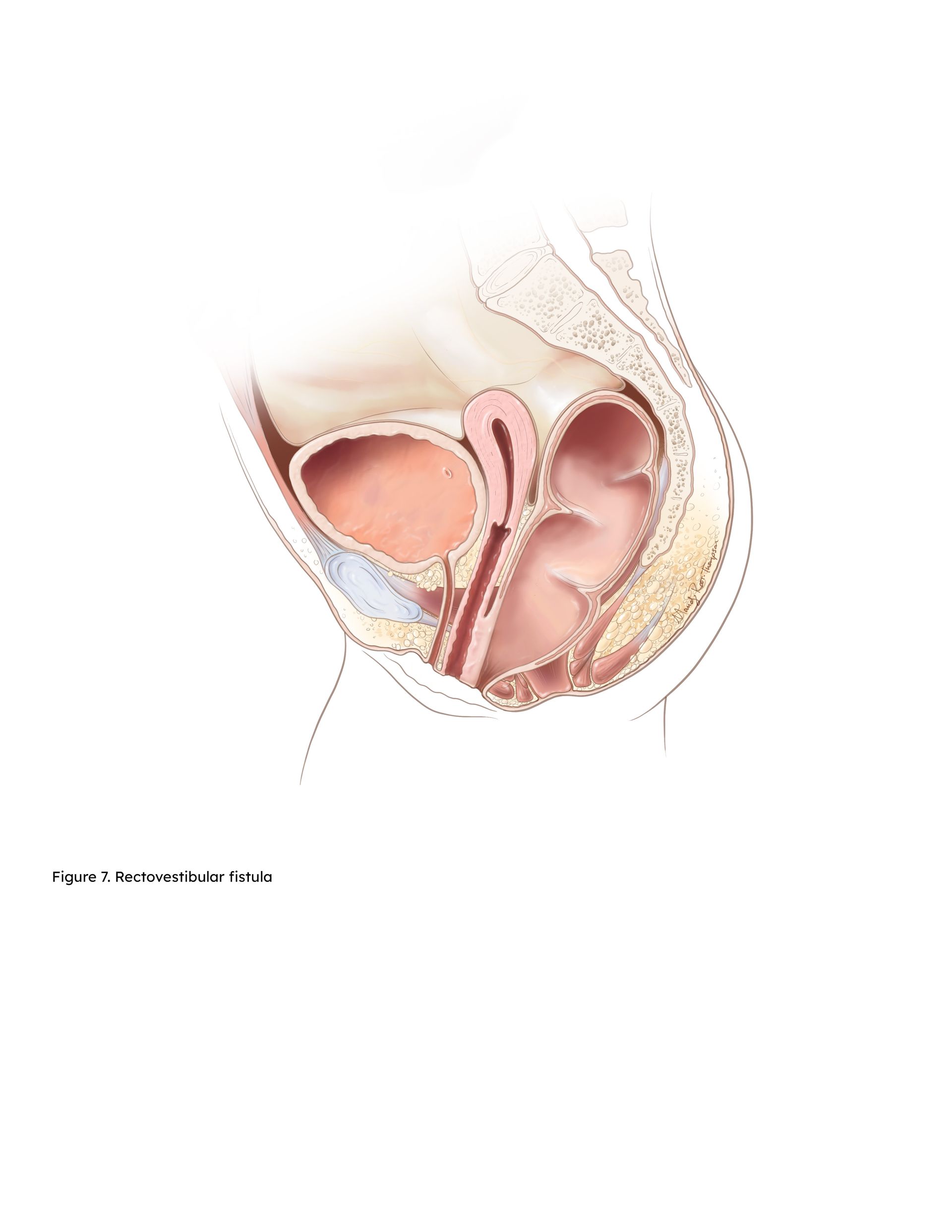
Slide title
Rectovestibular Fistula
Button
Slide title
Variations of the Distal Rectum (Female)
Button