Colorectal Quiz: August 28, 2023
Quiz for August 21:
A baby girl with ARM and rectovestibular fistula is taken to the OR for planned PSARP. Careful inspection reveal at first a normal appearing introitus and hymen, but probing shows that in fact she has distal vaginal atresia. What would you do in this case? Some potential options are below.
a. Cancel the procedure and come back another day
b. Proceed with PSARP and leave the vagina for another day
c. Proceed with PSARP and perform laparoscopy to determine the Mullerian anatomy
d. Proceed with PSARP and perform vaginal replacement using the distal rectum left for neovagina and mobilize a more proximal piece of rectum for the anoplasty
e. Proceed with PSARP using the rectum in the vestibule for rectum and performing a neovagina with sigmoid or small bowel
f. Something not listed above, in such a case I would________________________________.
Answer for August 21st:
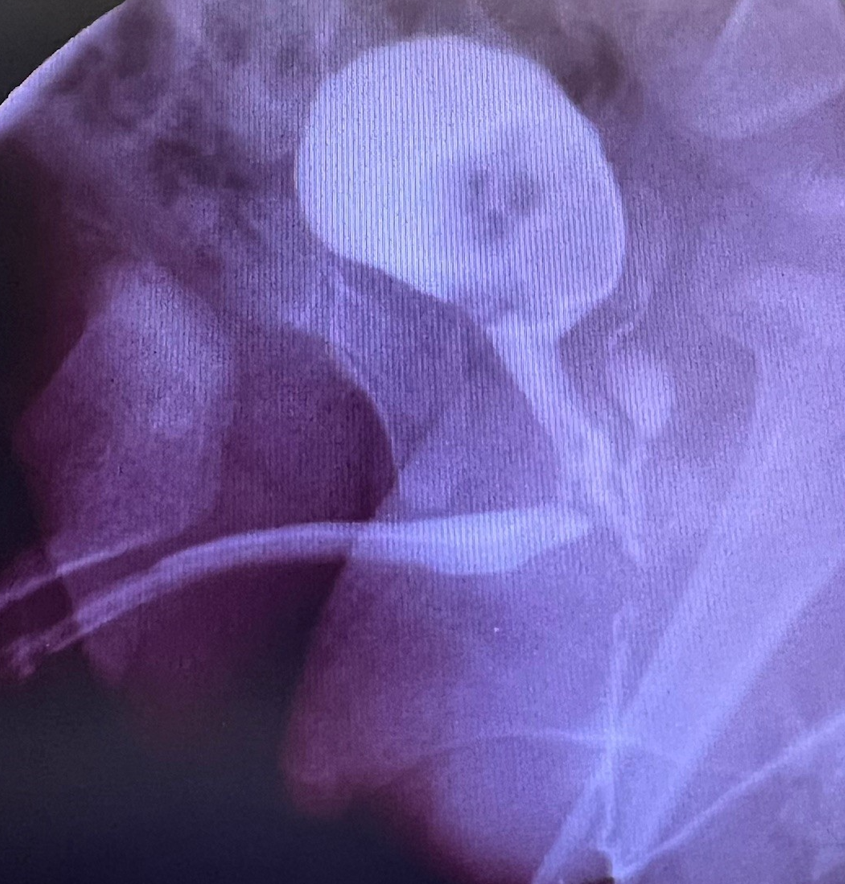
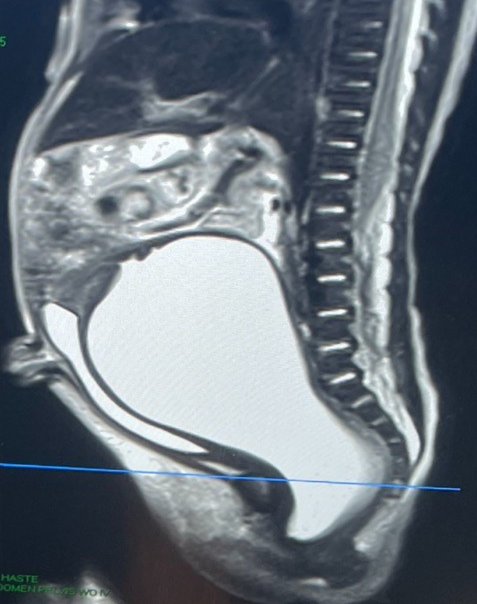
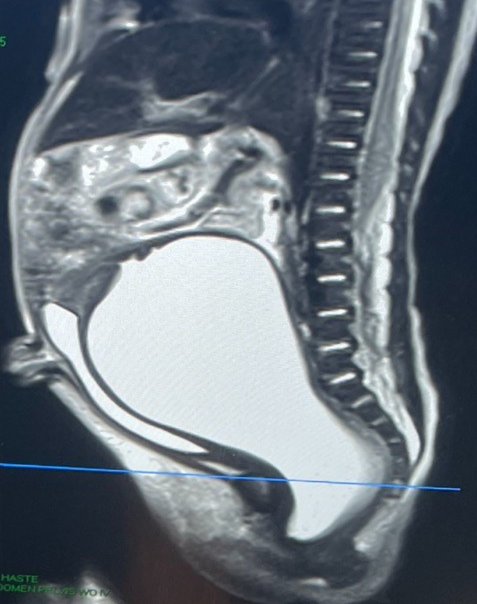
This is a fascinating case and reminds us of how important it is to always assess the Mullerian anatomy in any female patient with ARM. We decided to perform the PSARP and to do a diagnostic laparoscopy. (Choice C). The laparoscopy revealed an atretic left Mullerian system with normal ovary, and what appeared to be a unicornuate uterus on the right with potentially a blind ending distal vagina in the pelvis. To continue this case, the next quiz is – what would you do now?
Quiz for August 28th:
Based on last week’s quiz, a baby girl with ARM and rectovestibular fistula who was taken to the OR for a PSARP and found to have distal vaginal atresia – with laparoscopy performed showing an atretic left Mullerian system with normal ovary, and what appeared to be a unicornuate uterus on the right with potentially a blind ending distal vagina in the pelvis. What would you do now?
A. PSARP only, leave the Mullerian system untouched
B. PSARP plus vaginal replacement using the distal rectum
C. PSARP plus vaginal replacement using sigmoid, keep the distal rectum as rectum
D. Pull-through of native left vagina to perineum
E. Something not listed above, I would do___________________________.
How would you handle this case?