Colorectal Quiz: January 9, 2023
Last week I asked you about a Hirschsprung’s challenge:
A patient with total colonic HD has been living their life with an ileostomy, but they are short gut – requiring 12 hours of TPN plus enteral feeds via a G tube. They are being evaluated for a possible small bowel transplant. Is there anything to be done for this patient to improve their nutrition?
Many of you seemed puzzled about this case. This is a rare circumstance but there are two key things to do. First – make sure you know their urine sodium, and if low (less than 20 mmol/L) they need oral sodium supplementation which will help with their nutrition (by increasing glucose absorption). The second issue involves the distal bowel – there is small bowel and colon with HD in it that is dysfunctional, and can cause a low-grade enterocolitis. In my view in such cases that are behaving short gut, they need to become the best possible short gut patient they can be, which means removal of the distal bowel, and leaving a short Hartman’s of the rectum. Prior to doing this we confirmed with mapping, and biopsying of the small bowel and colon, that this was, in fact, total colonic HD.
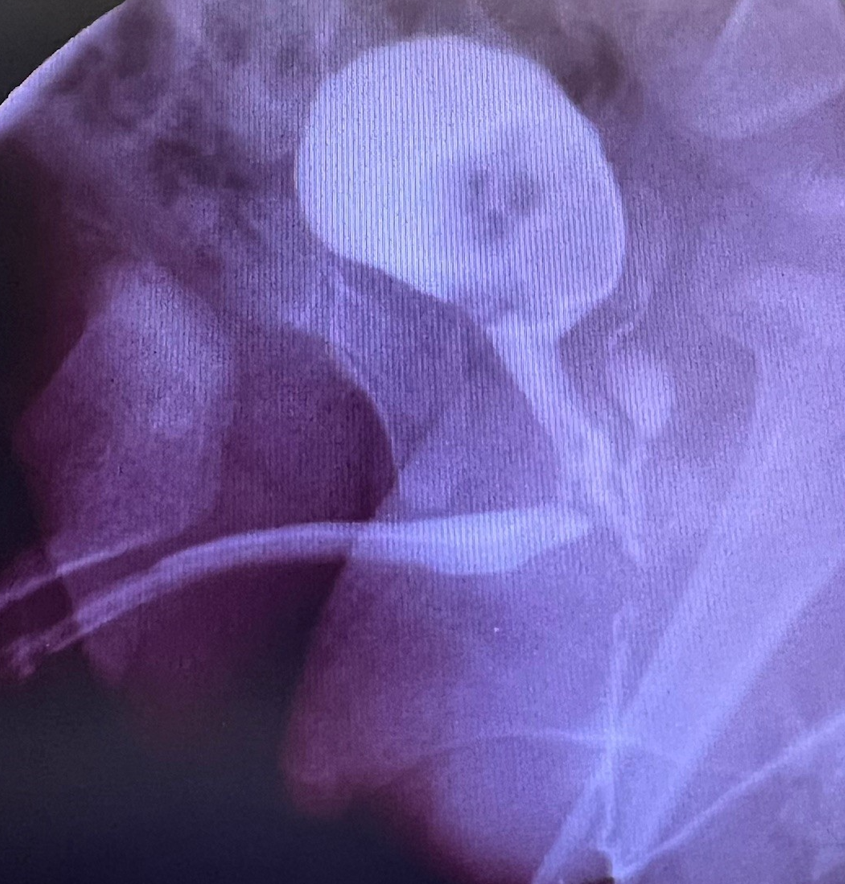
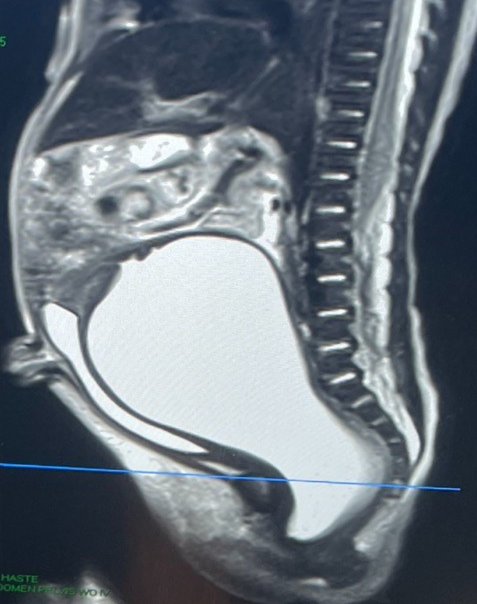
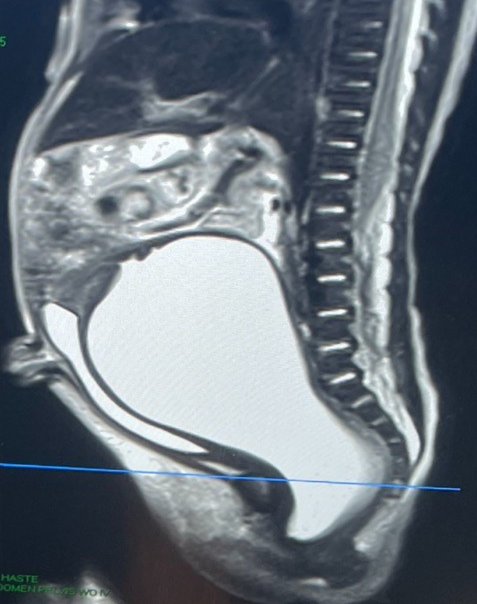
Ok, for this week, below are images of a male with ARM who underwent a newborn colostomy. From these images can you tell:
- Is there enough distal rectum for the pull-through?
- Can this be done by PSARP or will this need laparoscopy/laparotomy?
- What is the potential of bowel control?
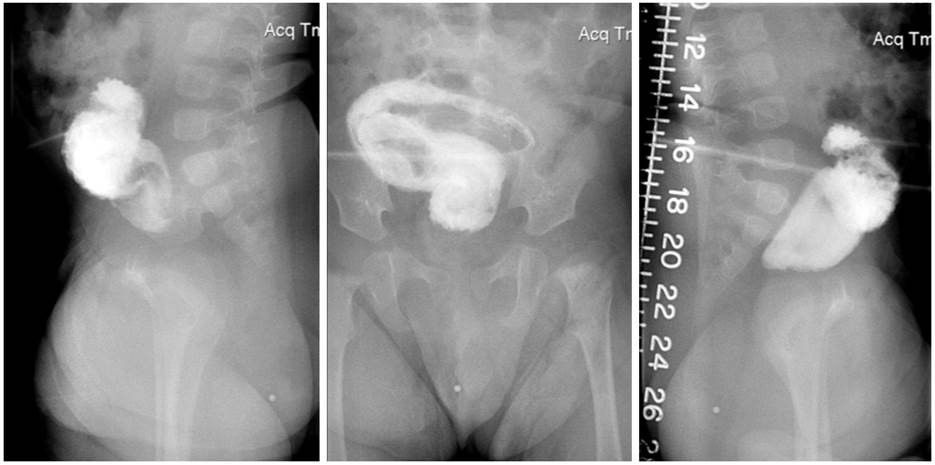
How would you handle this case?
New Paragraph